Medicare Advantage Plans
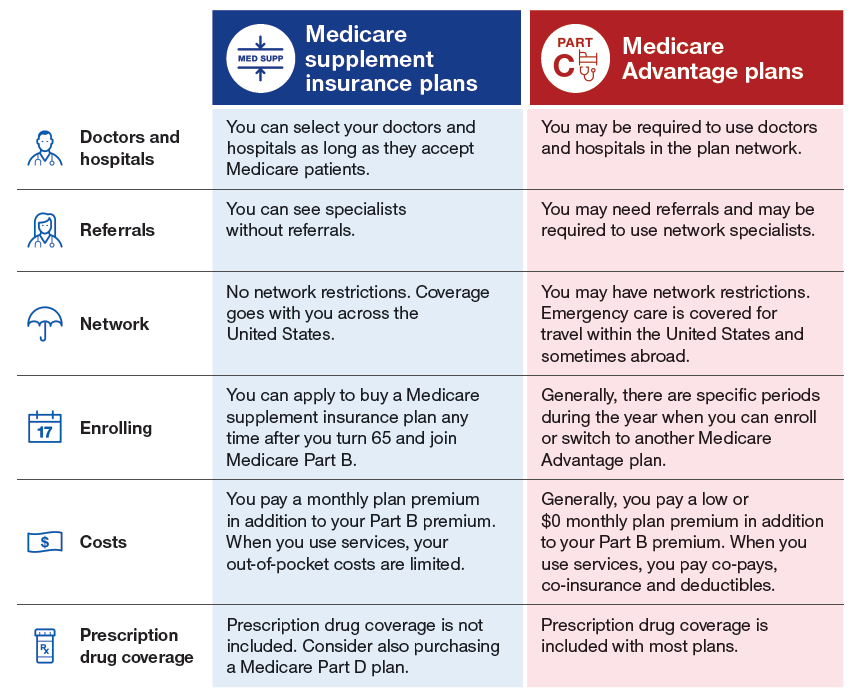
What are Medicare Advantage Plans?
A Medicare Advantage Plan is another way to get your Medicare coverage. Medicare
Advantage Plans, sometimes called “Part C” or “MA Plans,” are offered by Medicare-approved private companies that must follow rules set by Medicare. If you join a
Medicare Advantage Plan, you’ll still have Medicare but you’ll get most of your
Medicare Part A (Hospital Insurance) and Medicare Part B (Medical Insurance)
coverage from the Medicare Advantage Plan, not Original Medicare.
How do Medicare Advantage Plans work?
When you join a Medicare Advantage Plan, Medicare pays a fixed amount for your
coverage each month to the company offering that plan. These companies must
follow Medicare’s coverage rules. Medicare Advantage Plans have yearly contracts
with Medicare. The plan must notify you about any changes before the start of the
next enrollment year. If you join a Medicare Advantage Plan, you’ll have all of the same rights and protections that you would have under Original Medicare.
What’s covered?
Medicare Advantage Plans cover all Part A and Part B services. However, if you’re
in a Medicare Advantage Plan, Original Medicare will still cover the cost for hospice
care, some new Medicare benefits, and some costs for clinical research studies. In all
types of Medicare Advantage Plans, you’re always covered for emergency and urgent
care. Some Medicare Advantage Plans offer extra coverage, for things like vision, hearing,
dental, and other health and wellness programs. Plans have a yearly limit on what
you pay out-of-pocket for Part A and Part B covered services. Once you reach your
plan’s limit, you’ll pay nothing for Part A and Part B covered services for the rest of
the year.
Prescription drug coverage
Most Medicare Advantage Plans include Medicare prescription drug coverage
(Part D). In certain types of plans that don’t include drug coverage (like Medical
Savings Account Plans and some Private-Fee-for-Service Plans), you can join a separate
Medicare Prescription Drug Plan.
